Your Daily Meds - 7 December, 2022
Good morning and welcome to your Wednesday dose of Your Daily Meds.
Bonus Review: In massive haemorrhage, there is redistribution of the cardiac output. Which organs receive less blood flow? Which organs have maintained blood supply?
Answer: With redistribution of the cardiac output, we see -
Peripheral vasoconstriction - reduced perfusion to skin and muscles
Renal vasoconstriction - Remember normally 25% of the cardiac output goes to the kidneys, which is much more than is needed for oxygen delivery to the organ; oliguria will result and decrease total body fluid loss
Cerebral blood flow is maintained preferentially - the maintenance is achieved by mechanisms involving the carotid sinus reflex, pressure autoregulation, metabolic autoregulation
Anatomy Case:
Let’s dive in to the Right Upper Quadrant.
Since you are all going to be asked to do this at some point, we might as well get it out of the way:
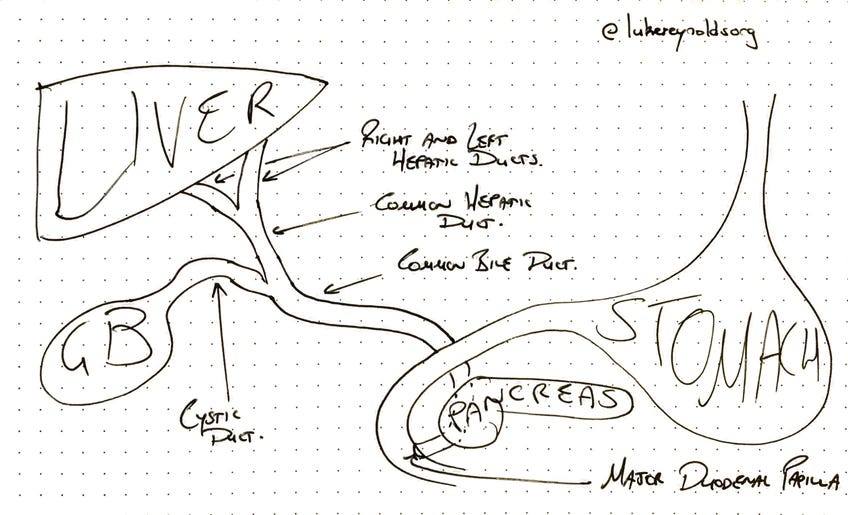
*(Puts on annoyed Surgeon voice)* “Draw the extra-hepatic biliary tree on that whiteboard over there.”
“And while you’re at it, tell me how cholelithiasis is different from choledocholithiasis!”
Stop now, quickly scribble some tube-like structures on a piece of paper, block some of those tubes with some scribbled stones, and meet me further down.
Case:
You are an intern on the surgical ward.
Your first patient is Bob Jones, a 45-year-old male who weighs approximately 70kg. He has been kept nil by mouth due to a small bowel obstruction. He will require maintenance fluids while on the ward.
The next patient is Tammy Collins, a patient admitted with a provisional diagnosis of gastritis and who was just flagged to you by the nurses as being quite unwell overnight.
On examination, Tammy is:
Pale and diaphoretic
Pulse rate of 125
Blood pressure of 100/62
Febrile
Peritonitic with rigidity and involuntary guarding of the abdomen
You urgently call your Registrar, and are requested to write up a STAT dose of fluids for the Tammy while she is on her way.
Pause now and think what your respective fluid orders will be for these two patients. Justify your choices as if to an examiner.
Back to the Biliary Tree:
Righto, you should able to scribble something resembling my effort below:
Then for cholelithiasis, you should scribble a stone into the gallbladder or cystic dust. And for choledocholithiasis, whack a stone somewhere into the common bile duct.
Then calmly turn from the whiteboard and ask “will that be all?”…
(Extra points for drawing the ampulla of Vater and sphincter of Oddi.)
(Feel free to name an anatomical feature after yourself while you are there…)
Meanwhile on your Fluid Round:
For Bobby:
Assuming no other pressing medical concerns or electrolyte derangements
Two 1L bags of IV 0.3% sodium chloride and 3.3% glucose with 40mmol of potassium at 83mL/h (1L, 12 hourly) would be sufficient to meet the daily (24 hour) requirements of a 70kg adult
25-30 mL/kg/day (based on ideal body weight) of water
1-2 mmol/kg/day sodium, potassium, chloride
50-100g/day glucose
BUT his bowel obstruction is almost certainly going to cause some third spacing
Patients with third spacing may require replacement fluids on top of their maintenance as well as close monitoring of electrolytes - especially++ potassium.
Different fluids, such as 0.9% normal saline with potassium, 0.18% sodium chloride and 4% glucose, and other combinations; and different rates, such as 62, 100 or 125 ml/hour should be justified but may be acceptable.
I’m somewhat partial to normal saline with 20-40 mmol Potasium at a rate titrated to urine output and clinical findings - dictating litres (bags) per day
Incorrect answers would include high volume saline only, such as 1L 0.9% saline over one or two hours; or blood.
Extra points for mentioning regular monitoring of electrolytes (even twice per day) and maintaining a urine output of at least 0.5mL/kg/hr.
Extra extra points for mentioning a fluid balance chart - urine, nasogastric output versus fluids in etc.
Extra extra extra points for mentioning the utility of a daily shot of albumin to play with intravascular colloid osmotic pressure - would be dictated by surgeon’s preference, however.
For Tammy, on the other hand:
She is shocked with a surgical abdomen, on the background of gastritis, concerning for gastric perforation
Now the decision is much easier
She needs 0.9% Normal Saline 20mL/kg as a STAT pushed administration
Practically, this means request 1L of Saline “right now please” at the fastest rate possible, then titrate to physiological response and wait for the cavalry to arrive
Slow rates of infusion, with maintenance fluids such as 0.33% or 0.18% sodium chloride solution, are not suitable for this acute resuscitation situation
Colloids, such as 4% albumin, may come into the story later, but not in the acute fluid resuscitation phase of a shocked patient
Extra points for mentioning ABCs, large bore cannulae etc
Extra extra points for thinking about taking some blood for haemoglobin, lactate, coats, cross-match and group and hold…
Bonus: What are some delayed responses to major blood loss?
Answer in tomorrow’s dose.
News: I made a little Ward Call Course for you all. It maps out an Evening Ward Call shift and covers a bunch of common tasks that you may need to do, like:
Deteriorating Patients
Heparin Infusions
Fluid Orders
Electrolyte Replacement
Difficult patients - Discharge Against Medical Advice, Ryan’s Rule
End of Life etc
You can find the course page here:
It’s free and always will be. Let me know what you think.
Remember, you are free to rip these questions and answers and use them for your own flashcards, study and question banks.
As always, please contact me with any questions, concerns, tips or suggestions. Have a great day!
Luke.