Your Daily Meds - 5 December, 2022
Good morning and welcome to your Monday dose of Your Daily Meds.
Case:
You are working on a general medicine ward and are asked to review the following chest x-ray of a 70-year-old male with orthopnoea:
Your job is to:
Systematically interpret the CXR as if you were going to report to an examiner.
Think of a provisional and differential diagnoses.
Then think of a general approach to management for the provisionally diagnosed condition.
Emergency:
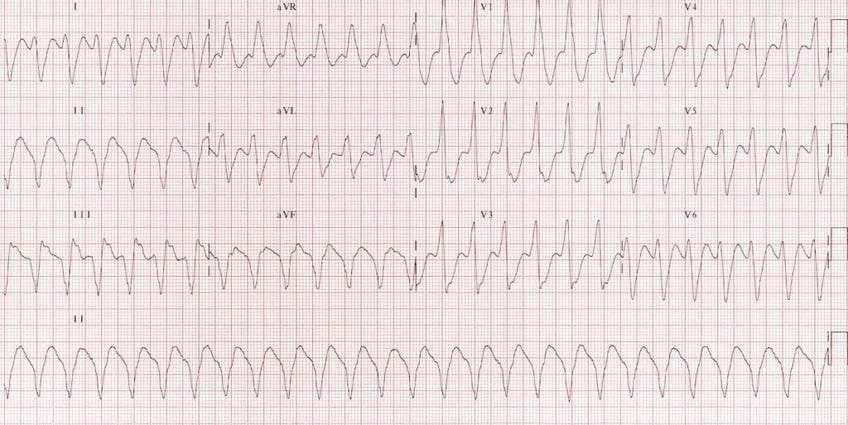
So you are in the Emergency Department when A 75-year-old male is brought in complaining of palpitations. You are handed the following ECG:
Which of the following best describes the ECG?
Sick sinus syndrome
Sinus tachycardia
Narrow complex tachycardia
Wide complex tachycardia
Atrial flutter
Have a think, and meet me further down for the answer.
Case Discussion:
Basically, this is a case of Congestive Cardiac Failure.
Imaging Findings:
You should have a basic model for CXR interpretation. Consider the ABCs as a useful approach. But in this case, important findings include:
Cardiomegaly
Cephalisation of pulmonary veins
Pulmonary interstitial oedema
Increased hilar markings of central pulmonary venous congestion
Differential Diagnoses:
Congestive Cardiac Failure/Heart Failure
Pneumonia
Pleural Effusion
Atelectasis
Or other reasonable DDx
Principles of Management:
If the patient needs acute therapy: as per DRSABCDE.
Short-term symptomatic management may require upright positioning, reduction of pre-load, diuresis and some positive pressure ventilation or high flow oxygen delivery - but this is not an emergency case, the setting is on a ward.
Differentiate between HFpEF and HFrEF: Echocardiogram.
Angiotensin-converting enzyme (ACE) inhibitors, angiontensin II receptor blockers (ARBs), beta-blockers such as bisoprolol and metoprolol, along with spironolactone, have been shown to be of mortality benefit in patients with HFrEF.
Symptomatic benefit with no clear mortality benefit would include other diuretics, nitrates, digoxin and hydralazine.
Include a discussion of a multidisciplinary approach - lifestyle modification, fluid restriction, pharmacological therapy, allied health input and potential surgical input pending any spectacular echocardiogram findings.
Returning to the Emergency Department:
Answer: Wide complex tachycardia.
The ECG can be described as wide complex tachycardia as there is tachycardia (>100 bpm) and a wide QRS-complex (>120 ms). The differential diagnosis for wide complex tachycardias includes ventricular tachycardia, wide complex supraventricular tachycardia, accelerated idioventricular rhythms, pacemaker rhythms and even ventricular fibrillation. Note that hyperkalaemia and bundle branch blocks can contribute to wide QRS complexes as well, just not necessarily the tachycardia.
So no clear P waves of sinus tachycardia, nowhere near narrow complex QRSs and no sawtoothing.
It is good to have a system for ECG interpretation. Try LITFL for an epic ECG primer.
Bonus: Imagine you suddenly remove 1L of blood volume from an unlucky patient. What compensatory processes might occur in that patient to maintain effective blood volume, cardiac output and arterial blood pressure?
Answer in tomorrow’s dose.
News: I made a little Ward Call Course for you all. It maps out an Evening Ward Call shift and covers a bunch of common tasks that you may need to do, like:
Deteriorating Patients
Heparin Infusions
Fluid Orders
Electrolyte Replacement
Difficult patients - Discharge Against Medical Advice, Ryan’s Rule
End of Life etc
You can find the course page here:
It’s free and always will be. Let me know what you think.
Remember, you are free to rip these questions and answers and use them for your own flashcards, study and question banks.
As always, please contact me with any questions, concerns, tips or suggestions. Have a great day!
Luke.